Introduction
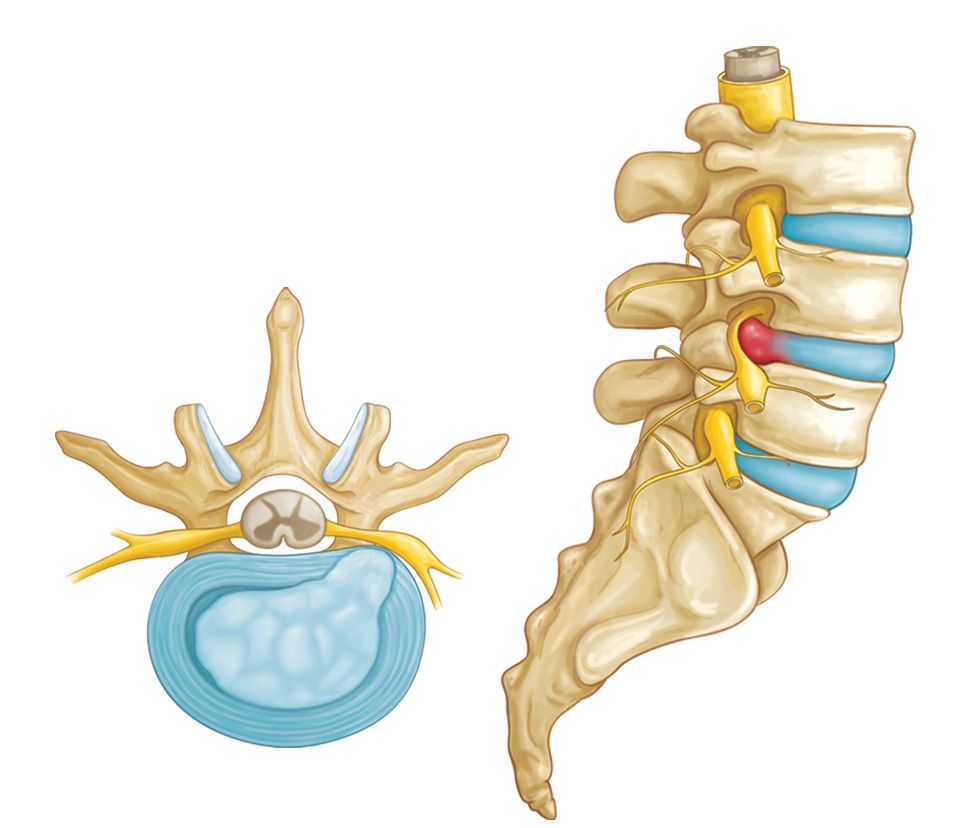
In the spine, a disc or a nucleus pulposus is localized between vertebral bodies. It supports the spine by acting as a shock-absorbing cushion. A herniated disc in the spine is a condition during which a nucleus pulposus is displaced from intervertebral space. In some instances, a herniated disc can compress the nerve or the spinal cord that causes pain consistent with nerve compression or spinal cord dysfunction also known as myelopathy.
An intervertebral disc is composed of annulus fibrous which is a dense collagenous ring encircling the nucleus pulposus. Disc herniation occurs when part or all the nucleus pulposus protrudes through the annulus fibrous. The most common cause of disc herniation is a degenerative process in which as humans age, the nucleus pulposus becomes less hydrated and weakens. This process will lead to progressive disc herniation that can cause symptoms. The second most common cause of disc herniation is trauma. Other causes include connective tissue disorders and congenital disorders such as short pedicles. Disc herniation is most common in the lumbar spine followed by the cervical spine. The incidence of herniated disc is about 5 to 20 cases per 1000 adults annually and is most common in people in their third to the fifth decade of life, with a male to female ratio of 2:1.
Treatment / Management
Acute cervical and lumbar radiculopathies due to herniated disc are primarily managed with non-surgical treatments. NSAIDs and physical therapy are the first-line treatment modalities. Translaminar epidural injections and selective nerve root blocks are the second line modalities. These are good modalities for managing disabling pain. Patients who fail conservative treatment or patients with neurological deficits need timely surgical consultation.

Reference
Scott C. Dulebohn; Ruben Ngnitewe Massa; Fassil B. Mesfin.